Opioid Use Disorder in the United States
Photo by Towfiqu barbhuiya from Pexels
By Macy Holmgren
Published Winter 2023
Special thanks to Robyn Mortensen and Jamie LeSeur for editing and research contributions.
Summary+
Opioid use disorder affects 16 million people worldwide and over 2.1 million in the United States. OUD has been an ever-growing public health issue in the nation since 1999, causing death on an unprecedented scale through 2022. Chronic pain, overprescription, illicit use of prescription opioids, and inability to access treatment are all contributors to OUD and are perpetuated throughout the nation. Victims of opioid use disorder have a higher chance of becoming addicted to harder drugs, experiencing medical complications, and dying from an overdose. Evidence-based practices such as medication-assisted treatment must be leveraged to address the issue and reduce the number of overdose casualties the nation experiences. Increasing access to medication-assisted treatment can improve overall mortality rates and the quality of life in OUD patients.
Key Takeaways+
- Opioid use disorder is a public health issue in the United States and has led to many unnecessary deaths between 1990–2022.
- Chronic pain, overprescription, illicit use of opioids, and an inability to access effective treatment are all contributing factors to the ever-rising issue of OUD in the US.
- Opioids can be a gateway drug to other harder drugs, such as heroin. Additionally, medical complications and death are all potential consequences for OUD patients.
- It can be difficult for patients to receive the care they need due to systematic issues like a lack of doctors that are willing and able to prescribe medication-assisted treatments for their patients.
- A best practice for OUD is medication-assisted treatment, which uses a system of FDA-approved medication combined with behavioral therapy to assist in OUD recovery.
- Greater access to MAT could improve the OUD mortality rate in the US.
Key Terms+
Non-medical opioid use—Taking prescribed or diverted prescription drugs (drugs not prescribed to the person using them) not in the way, for the reasons, in the amount, or during the period prescribed.1
Opioid—A class of drugs naturally found in the opium poppy plant. They cause users’ brains to produce a variety of effects, including the relief of pain by blocking pain signals between the brain and the body.2 Doctors sometimes prescribe them to treat persistent or severe pain, and they can be highly addictive.3 Examples of opioids include heroin, morphine, codeine, fentanyl, and synthetic opioids such as oxycodone.4
Opioid overdose—Opioids affect the part of the brain that regulates breathing. When people take high doses of opioids, the body cannot process the drug in such concentration and will slow or completely stop breathing. Without medical intervention, an overdose will lead to death.5
Opioid use disorder (OUD)—An addiction to opioids that is chronic and lifelong with serious potential consequences such as disability, relapse, and even death.6 OUD is listed in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) as a problematic pattern of opioid use leading to problems or distress.7 Physical dependence occurs within 4–8 weeks, much shorter than other substance use disorders. Ease of access is a notorious reason for the epidemic in the United States.8 OUD is typically measured through overdose rates versus the number of people it affects. “Opioid use disorder” is preferred over other terms such as “opioid abuse,” “opioid addiction,” or “opioid dependence.”9
Persistent opioid use—When a patient fills at least one opioid prescription 90–365 days after surgery to aid with chronic pain. These patients are typically more at risk for opioid use disorder than patients who did not fill at least one opioid prescription in the days after surgery.10
Substance use disorder—A treatable, chronic disease characterized by a problematic pattern of use of a substance leading to noticeable impairment or distress.11 This may include alcohol, cannabis, hallucinogens, tobacco, stimulants, and opioids.
Context
Q: What is opioid use disorder?
A: Opioid use disorder An addiction to opioids that is chronic and lifelong with serious potential consequences such as disability, relapse, and even death.6 OUD is listed in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) as a problematic pattern of opioid use leading to problems or distress.7 Physical dependence occurs within 4–8 weeks, much shorter than other substance use disorders. Ease of access is a notorious reason for the epidemic in the United States.8 OUD is typically measured through overdose rates versus the number of people it affects. “Opioid use disorder” is preferred over other terms such as “opioid abuse,” “opioid addiction,” or “opioid dependence.”9 (OUD) is the chronic use of opioids that causes clinically significant distress or impairment. This disorder can develop if a person takes prescription opioids in a way that is not prescribed, takes someone else’s prescription, or takes opioids to “get high.”12 Most prescribed opioids are pills meant to be taken orally. However, people sometimes misuse opioids by crushing the pills or opening the capsules, dissolving the opioid powder in water, or injecting the liquid into a vein. Snorting is also a common method of misuse.13, 14
Medical professionals diagnose OUD An addiction to opioids that is chronic and lifelong with serious potential consequences such as disability, relapse, and even death.6 OUD is listed in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) as a problematic pattern of opioid use leading to problems or distress.7 Physical dependence occurs within 4–8 weeks, much shorter than other substance use disorders. Ease of access is a notorious reason for the epidemic in the United States.8 OUD is typically measured through overdose rates versus the number of people it affects. “Opioid use disorder” is preferred over other terms such as “opioid abuse,” “opioid addiction,” or “opioid dependence.”9 based on the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5), which defines OUD as the person’s desire to obtain and take opioids despite social and professional consequences.15 Other diagnostic criteria include unsuccessful efforts to cut down or control use and failure to fulfill personal obligations.16
Opioid use disorder An addiction to opioids that is chronic and lifelong with serious potential consequences such as disability, relapse, and even death.6 OUD is listed in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) as a problematic pattern of opioid use leading to problems or distress.7 Physical dependence occurs within 4–8 weeks, much shorter than other substance use disorders. Ease of access is a notorious reason for the epidemic in the United States.8 OUD is typically measured through overdose rates versus the number of people it affects. “Opioid use disorder” is preferred over other terms such as “opioid abuse,” “opioid addiction,” or “opioid dependence.”9 is a type of substance use disorder A treatable, chronic disease characterized by a problematic pattern of use of a substance leading to noticeable impairment or distress.11 This may include alcohol, cannabis, hallucinogens, tobacco, stimulants, and opioids. but is classified as its own disorder. OUD can lead to other types of substance use disorders, such as alcohol, tobacco, hallucinogen, cannabis, and stimulant use disorder.17 For this brief, OUD rates will be measured primarily through opioid overdose Opioids affect the part of the brain that regulates breathing. When people take high doses of opioids, the body cannot process the drug in such concentration and will slow or completely stop breathing. Without medical intervention, an overdose will lead to death.5 , which according to the CDC, is when “too much of the drug overwhelms the brain and interrupts the body’s natural drive to breathe.”18 Opioid overdose will typically cause death 1–3 hours after taking the overdosing quantity of the drug.19 It is possible, but difficult, to reverse an overdose.20 For the purpose of this brief, “opioid overdose” will refer to overdoses that cause death and those that do not.
Q: How did the opioid epidemic begin?
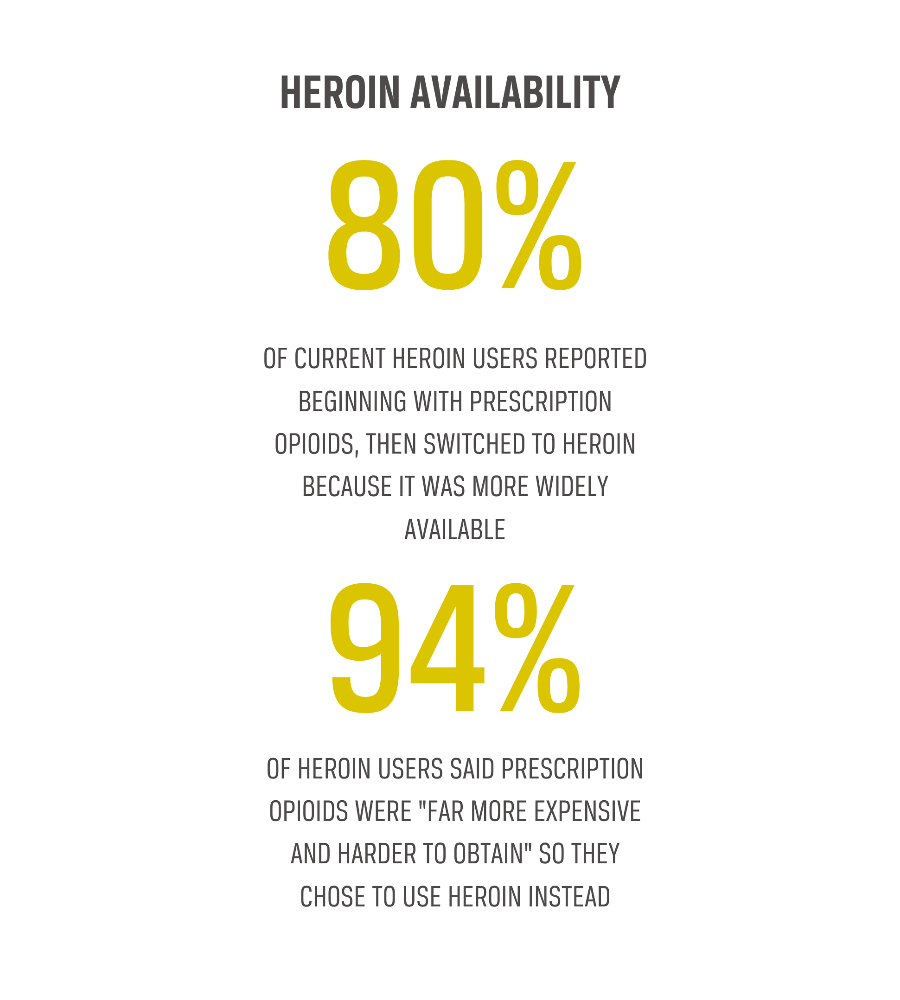
A: Before 1999, hardly any opioids were prescribed as an effective method of pain relief.21 A large number of patients have been prescribed opioids since then, followed by an increase in opioid overdose Opioids affect the part of the brain that regulates breathing. When people take high doses of opioids, the body cannot process the drug in such concentration and will slow or completely stop breathing. Without medical intervention, an overdose will lead to death.5 deaths over the following 20 years, as recorded by the CDC.22 A reported 3,442 people died from opioid overdose in 1999.23 One calculation shows that from 2013–2019, death rates related to opioids increased by 1,040%.24 Out of all 70,630 drug-related deaths in 2019, 49,860 (70.6%) of those involved an opioid.25 Just 5 years earlier, in 2014, 61% of all 47,055 drug-related deaths involved an opioid.26 In previous years, opioid-related overdoses mostly involved prescription opioids, but today illicit and synthetic opioids such as fentanyl and heroin are beginning to increase in number in the US.27 Compared to rates from 1999, synthetic opioid overdoses were 97 times more common in 2021. For comparison, prescription opioid overdoses were cited to be 4.9 times more common since 1999.28 There is a significant relationship between the two types of opioids: prescribed opioids are cited as a major gateway to illicit opioid use—4 out of 5 heroin users report that they began with prescription opioids before moving to heroin.29
Q: Who is most affected by OUD?
A: Across the United States, opioid use disorder An addiction to opioids that is chronic and lifelong with serious potential consequences such as disability, relapse, and even death.6 OUD is listed in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) as a problematic pattern of opioid use leading to problems or distress.7 Physical dependence occurs within 4–8 weeks, much shorter than other substance use disorders. Ease of access is a notorious reason for the epidemic in the United States.8 OUD is typically measured through overdose rates versus the number of people it affects. “Opioid use disorder” is preferred over other terms such as “opioid abuse,” “opioid addiction,” or “opioid dependence.”9 and overdose disproportionately affect people who are white, male, and middle-aged.30 Socioeconomic groups with a higher risk of OUD include low-income individuals, those who experience homelessness and insecure housing, and people who did not graduate from high school or experienced a divorce.31 Individuals aged 18–25 years old have the greatest non-medical use of opioids in the past year, while the greatest use of prescription opioids is in adults aged 26 and older.32 Overall, OUD death rates are the highest among males under the age of 50.33 In addition, non-Hispanic white females experiencing homelessness have the highest risk of opioid overdose Opioids affect the part of the brain that regulates breathing. When people take high doses of opioids, the body cannot process the drug in such concentration and will slow or completely stop breathing. Without medical intervention, an overdose will lead to death.5, and non-Hispanic white males have the highest risk of an opioid-related emergency room visit.34 The Northeastern, Midwestern, and Southern regions of the United States are affected the most as well.35 Reasons for this regional disparity in opioid overdoses vary greatly and have deeper, systemic, and long-term roots than other regions in the United States.36
Q: Where is the opioid epidemic the worst?
A: OUD An addiction to opioids that is chronic and lifelong with serious potential consequences such as disability, relapse, and even death.6 OUD is listed in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) as a problematic pattern of opioid use leading to problems or distress.7 Physical dependence occurs within 4–8 weeks, much shorter than other substance use disorders. Ease of access is a notorious reason for the epidemic in the United States.8 OUD is typically measured through overdose rates versus the number of people it affects. “Opioid use disorder” is preferred over other terms such as “opioid abuse,” “opioid addiction,” or “opioid dependence.”9 affects over 16 million people worldwide, with over 2.1 million opioid-related deaths occurring in the United States, which is the highest in the world.37, 38 More opioids per capita are manufactured and prescribed in the United States than any other country in the world—in 2010, the number of opioids prescribed in the US peaked at 782 morphine milligram equivalents (MME) per capita and decreased in 2015 to 640 MME per capita.39, 40 Of all countries that experience issues with opioid use and overdose within their population, the United States has about 2.7 million deaths. Regionally, the highest rates of OUD are reported in New England, the Rust Belt, the Mountain region, and the South.41 A reported 215 million opioids were prescribed in 2006 in the US, which reduced to 142 million in 2020.42 Compared to the US, Canada is close behind in both opioid prescription and opioid-related deaths.43 Europe is less impacted by the opioid epidemic due to low prescription rates in general across the whole continent. Between 2007 and 2017, rates were at two opioid-related deaths per 100,000 population annually. In the US, rates were between 3 and 15 per 100,000 per year.44
Contributing Factors
Chronic Pain
Chronic pain contributes to the development of opioid use disorderAn addiction to opioids that is chronic and lifelong with serious potential consequences such as disability, relapse, and even death.6 OUDAn addiction to opioids that is chronic and lifelong with serious potential consequences such as disability, relapse, and even death.6 OUD is listed in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) as a problematic pattern of opioid use leading to problems or distress.7 Physical dependence occurs within 4–8 weeks, much shorter than other substance use disorders. Ease of access is a notorious reason for the epidemic in the United States.8 OUD is typically measured through overdose rates versus the number of people it affects. “Opioid use disorder” is preferred over other terms such as “opioid abuse,” “opioid addiction,” or “opioid dependence.”9 is listed in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) as a problematic pattern of opioid use leading to problems or distress.7 Physical dependence occurs within 4–8 weeks, much shorter than other substance use disorders. Ease of access is a notorious reason for the epidemic in the United States.8 OUD is typically measured through overdose rates versus the number of people it affects. “Opioid use disorder” is preferred over other terms such as “opioid abuse,” “opioid addiction,” or “opioid dependence.”9 because pain motivates people to seek the pain relief that opioids quickly provide. According to the CDC (which analyzed data from a 2016 National Health Interview Survey), about 20.4% of adults in the US experience chronic pain, with 8.0% experiencing chronic pain so debilitating that it limits their day-to-day activities.45 Some people with that kind of pain have reported that they need to take opioids just to maintain their pain level at a 10 (out of 10) and prevent it from going higher. Others report that they take opioids not to experience “euphoria” but to prevent “dysphoria.”46
Photo by Towfiqu barbhuiya on Unsplash
Approximately 60% of OUD patients who were seeking treatment for their abuse reported chronic pain and listed chronic pain as the reason for their initial use of an opioid.47 Imaging and genetic studies also suggest that diminished activity in the frontal cortex of the brain, which is induced by chronic pain, might be one factor that predisposes patients to OUD. While a significant body of research suggests that chronic pain can be a cause for the onset of OUD, patients also report comorbid chronic pain and OUD, making it unclear what came first in some instances.48 Nevertheless, chronic pain makes a person susceptible to chronic opioid use.49
In a study that randomly selected 10,000 battle-injured United States military personnel, 23.3% of the patients who survived 180 days past their discharge developed persistent opioid useWhen a patient fills at least one opioid prescription 90–365 days after surgery to aid with chronic pain. These patients are typically more at risk for opioid use disorder than patients who did not fill at least one opioid prescription in the days after surgery.10.50 After 8 years, the study followed up with these patients and found that 631 (6.8%) developed clinically recognized OUD. An association was found between injury severity and discharge opioid prescription amount and persistent opioid use after trauma. Persistent opioid use caused by chronic pain was associated with the long-term development of OUD.51
Overprescription
Overprescription of an opioid by a physician refers to prescribing in excess more often than is necessary for a patient to be relieved from pain.52 This contributes to the development of OUDAn addiction to opioids that is chronic and lifelong with serious potential consequences such as disability, relapse, and even death.6 OUD is listed in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) as a problematic pattern of opioid use leading to problems or distress.7 Physical dependence occurs within 4–8 weeks, much shorter than other substance use disorders. Ease of access is a notorious reason for the epidemic in the United States.8 OUD is typically measured through overdose rates versus the number of people it affects. “Opioid use disorder” is preferred over other terms such as “opioid abuse,” “opioid addiction,” or “opioid dependence.”9 because higher opioid prescription correlates with higher consumption by a patient.53 In cases where patients were prescribed an opioid for acute postoperative pain, about 90% of patients had leftover opioids 2 weeks after surgery. Most of these leftover opioids were not stored in a secure location.54 The effects of this study were not specifically measured to show how overprescription and poor storage influenced OUD, but there are many studies that show that these two practices make prescription opioids potentially available for diversion—when opioids are prescribed for one person but taken by another—and misuse.55, 56, 57
Physicians are the number one prescriber of opioids, followed closely by dentists, prescribing 15% and 12% of all opioids in the US, respectively.58 Compared to other countries with similar dental practices, US dentists proportionally prescribe opioids approximately 37 times more frequently. In an analysis of dental visits in which opioids were prescribed for acute pain in the US from 2011 to 2015, 29% of those opioids exceeded the MME-recommended limit for acute pain of 100 milligrams per day. Half of these total prescriptions from dentists exceeded the sufficient limit to treat typical oral pain of 3 days.59 Overprescription by a physician can, in turn, lead to opioid dependence in a patient and perpetuate OUDAn addiction to opioids that is chronic and lifelong with serious potential consequences such as disability, relapse, and even death.6 OUD is listed in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) as a problematic pattern of opioid use leading to problems or distress.7 Physical dependence occurs within 4–8 weeks, much shorter than other substance use disorders. Ease of access is a notorious reason for the epidemic in the United States.8 OUD is typically measured through overdose rates versus the number of people it affects. “Opioid use disorder” is preferred over other terms such as “opioid abuse,” “opioid addiction,” or “opioid dependence.”9 as a growing issue in the US.
From 2007 to 2012, 4.2 billion prescriptions were dispensed by pharmacies in the US and long-term care facilities. Of these 4.2 billion prescriptions, 289 million (6.8%) were opioids.60 Male and young adult patients are most impacted by overprescribing and are, therefore, at a higher risk of substance use and opioid-related death.61 With new restrictions and heightened awareness of their highly addictive properties, opioid prescriptions have declined from 257.9 million to 143.4 million (44.4%) from 2007 to 2021. However, overdoses continue to occur at heightened rates.62 Although overprescription rates have recently decreased, overprescription greatly contributed to the rise of OUDAn addiction to opioids that is chronic and lifelong with serious potential consequences such as disability, relapse, and even death.6 OUD is listed in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) as a problematic pattern of opioid use leading to problems or distress.7 Physical dependence occurs within 4–8 weeks, much shorter than other substance use disorders. Ease of access is a notorious reason for the epidemic in the United States.8 OUD is typically measured through overdose rates versus the number of people it affects. “Opioid use disorder” is preferred over other terms such as “opioid abuse,” “opioid addiction,” or “opioid dependence.”9 in the United States from the mid-1990s to the early 2000s and started a wave of opioid addiction that continues to affect many Americans.
Non-medical use of prescription opioids
Non-medical use of prescription opioids also contributes to the development of OUDAn addiction to opioids that is chronic and lifelong with serious potential consequences such as disability, relapse, and even death.6 OUD is listed in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) as a problematic pattern of opioid use leading to problems or distress.7 Physical dependence occurs within 4–8 weeks, much shorter than other substance use disorders. Ease of access is a notorious reason for the epidemic in the United States.8 OUD is typically measured through overdose rates versus the number of people it affects. “Opioid use disorder” is preferred over other terms such as “opioid abuse,” “opioid addiction,” or “opioid dependence.”9 through attempts to relieve chronic pain. Non-medical use of prescription opioids refers to use without one’s own prescription or use simply in pursuit of the drug’s pleasurable effects. This can occur with people who were not explicitly prescribed the opioid, by either taking it from someone they know or from an unsecured location.63 In Canada, it was discovered that among people 15 years of age or older, the rate of non-medical use of opioids in 2011 was 3.2%. Also, among surveyed adolescents in grades 7–12, 18% said they had used an opioid as a pain reliever without a prescription in the past year.64 While these statistics are not from the United States, they give an estimate of how accessible opioids are even without a prescription for someone living in North America.
Photo by Diana Polekhina on Unsplash
Throughout the United States, a total of 36,450 deaths were drug-related in 2020. Of these deaths, 74.5% specified a drug—one or more prescription drugs were involved in 73.8% of those deaths, and 73.8% of those deaths from prescription drugs involved opioids.65 Regionally, between 2008–2009, non-medical use of prescription opioids ranged from 3.6% in Nebraska to 8.1% in Oklahoma, with the highest opioid sales rates clustered in the Southeast and the Northwest United States.66 Of 27 states with overdose death rates above the national rate, 21 (77.8%) had rates of non-medical use of prescription opioids above the national rate.67
Distribution of opioids for non-medical purposes also occurs among those who received an official prescription from their physician for chronic pain. About 20% of all participants in a study on opioid distribution reported they had ever distributed their prescribed medication to others, regardless of intention.68 Even so, those who abused these opioids believed that their behavior was safer than the behavior of those who use illicit drugs, such as heroin. This belief occurred because opioids were licensed by the medication authority, as opposed to illegal drugs.69
Inability to Access Treatment
Though the inability to access treatment does not directly contribute to the rise of OUDAn addiction to opioids that is chronic and lifelong with serious potential consequences such as disability, relapse, and even death.6 OUD is listed in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) as a problematic pattern of opioid use leading to problems or distress.7 Physical dependence occurs within 4–8 weeks, much shorter than other substance use disorders. Ease of access is a notorious reason for the epidemic in the United States.8 OUD is typically measured through overdose rates versus the number of people it affects. “Opioid use disorder” is preferred over other terms such as “opioid abuse,” “opioid addiction,” or “opioid dependence.”9 in the United States, it does prevent individuals from gaining the help that they need, thus perpetuating the already high rates of OUD.
Access to treatment for opioid use disorderAn addiction to opioids that is chronic and lifelong with serious potential consequences such as disability, relapse, and even death.6 OUDAn addiction to opioids that is chronic and lifelong with serious potential consequences such as disability, relapse, and even death.6 OUD is listed in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) as a problematic pattern of opioid use leading to problems or distress.7 Physical dependence occurs within 4–8 weeks, much shorter than other substance use disorders. Ease of access is a notorious reason for the epidemic in the United States.8 OUD is typically measured through overdose rates versus the number of people it affects. “Opioid use disorder” is preferred over other terms such as “opioid abuse,” “opioid addiction,” or “opioid dependence.”9 is listed in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) as a problematic pattern of opioid use leading to problems or distress.7 Physical dependence occurs within 4–8 weeks, much shorter than other substance use disorders. Ease of access is a notorious reason for the epidemic in the United States.8 OUD is typically measured through overdose rates versus the number of people it affects. “Opioid use disorder” is preferred over other terms such as “opioid abuse,” “opioid addiction,” or “opioid dependence.”9 in the United States is limited and oftentimes flawed because treatment resources are insufficient, and doctors often feel hesitant to prescribe comprehensive treatments.70 Physicians may feel this way because addiction treatment is separated from mainstream health systems, and OUD education for prescribers is often not required for health care providers in the US.71 Many treatments are inconsistent and not standardized, which sometimes causes physicians to feel hesitant to apply them. This is true of medication therapy and behavioral therapy.72
Access to Medication-Assisted Treatment (MAT)
Medication-assisted treatment is by far the most effective form of treatment for OUDAn addiction to opioids that is chronic and lifelong with serious potential consequences such as disability, relapse, and even death.6 OUD is listed in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) as a problematic pattern of opioid use leading to problems or distress.7 Physical dependence occurs within 4–8 weeks, much shorter than other substance use disorders. Ease of access is a notorious reason for the epidemic in the United States.8 OUD is typically measured through overdose rates versus the number of people it affects. “Opioid use disorder” is preferred over other terms such as “opioid abuse,” “opioid addiction,” or “opioid dependence.”9, even more so than behavioral therapy or medication treatment alone.73 It is a form of treatment that combines medication and behavioral therapies together.74 Medication-assisted therapy includes treatment through methadone, buprenorphine, and extended-release naltrexone—all of which are FDA-approved medications that have reduced the risk of overdose by 50% in OUD patients.75 In a study from researchers at NYU Grossman School of Medicine, 86.6% of people with OUD do not receive medication-assisted therapy (MAT).76 However, 96% of states had OUD rates higher than buprenorphine treatment capacity rates, and 75% of certified opioid treatment programs (OTP) operated at 80% capacity or more in 2012.77
These numbers demonstrate that OUD treatment programs do not have the capacity to manage the number of OUD cases in the US. According to researchers, this is partially due to a lack of qualified medical personnel that are willing to work in non-government-owned OUD programs and treatment facilities, even despite scientific evidence that MAT is a safe treatment that works well for many.78 Also, publicly funded organizations are less likely than privately-funded organizations to adopt medication for addiction treatment, which means that even fewer programs are using MAT.79
Photo by Karolina Grabowska
Another reason MAT remains difficult to access for OUDAn addiction to opioids that is chronic and lifelong with serious potential consequences such as disability, relapse, and even death.6 OUD is listed in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) as a problematic pattern of opioid use leading to problems or distress.7 Physical dependence occurs within 4–8 weeks, much shorter than other substance use disorders. Ease of access is a notorious reason for the epidemic in the United States.8 OUD is typically measured through overdose rates versus the number of people it affects. “Opioid use disorder” is preferred over other terms such as “opioid abuse,” “opioid addiction,” or “opioid dependence.”9 patients is because of the physician waiver. The US Food and Drug Administration (FDA) provides physicians with waivers that allow them to prescribe medications to treat OUD to a certain number of patients.80 These waivers require at least 8 hours of training to complete. Approximately 33,000 physicians have obtained this waiver—however, less than half of them offer medication as a form of treatment for their patients.81 There are several reasons why this may be, including liability reasons from receiving only the minimum 8 hours of training, as well as a lack of confidence to take on the care of patients with OUD and co-occurring mental illnesses or substance use disorders, which can make treatment more complicated.82 Therefore, it can be difficult to find enough physicians in the United States who are willing and able to provide effective medications for patients suffering from OUD.
Access to Methadone Clinics
While MAT is the most effective form of treatment for OUDAn addiction to opioids that is chronic and lifelong with serious potential consequences such as disability, relapse, and even death.6 OUD is listed in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) as a problematic pattern of opioid use leading to problems or distress.7 Physical dependence occurs within 4–8 weeks, much shorter than other substance use disorders. Ease of access is a notorious reason for the epidemic in the United States.8 OUD is typically measured through overdose rates versus the number of people it affects. “Opioid use disorder” is preferred over other terms such as “opioid abuse,” “opioid addiction,” or “opioid dependence.”9, methadone treatment is also used and can only be performed in methadone clinics, which are not federally qualified.83 Methadone treatment is known to improve an addict’s quality of life and lower the overall mortality rate from OUD. In a study done in Georgia, 4 of the 5 counties with the highest opioid overdoseOpioids affect the part of the brain that regulates breathing. When people take high doses of opioids, the body cannot process the drug in such concentration and will slow or completely stop breathing. Without medical intervention, an overdose will lead to death.5 death rates had no methadone clinic accessible within a 15-minute drive.84 However, there were federally qualified clinics within a 15-minute drive for more than 67% of the population in these counties. Ease of access to these treatment-specific clinics is limited, hence the need to expand different forms of treatment to other, more accessible clinics, especially in areas where opioid overdose death rates are high.85
Consequences
Pathway to Other Drugs
With the use of prescription opioids comes the inevitable consequence of these same people trying and becoming addicted to illicit opioids—the non-medical use of illegal drugs deriving from opiates, such as heroin and fentanyl.86 There were over 56,000 deaths involving synthetic opioids in 2020, an increase of over 56% since 2019, which was largely driven by an increase in fentanyl deaths.87 In 2020, overdose rates involving synthetic opioids were more than 18 times higher than in 2013.88 Of all states, Mississippi had the highest increase in synthetic opioid deaths between 2019–2020 of 55.1%, a 29.2% increase from the year prior.89, 90
About 80% of current heroin users reported that they began with prescription opioids and then switched to heroin because it was more widely available. In a recent survey of people in opioid treatment centers, 94% said prescription opioids were “far more expensive and harder to obtain,” so they chose to use heroin instead.91 This shift in purchasing habits caused heroin-involved overdose deaths to increase 3 times from 2010–2014 and continues to increase. Among whites aged 18–45, heroin-usage rates have gone up more than 2.5-fold from 2001–2011.92
Health Risks
Mental Health
Many individuals who are addicted to opioids experience a myriad of health effects and symptoms when they attempt to stop taking them, which can affect their mental health. Researchers have shown that 3 days of opioid discontinuation can lead some individuals to experience moderate depression, severe anxiety, and other health effects.93 In this particular study, it took 10 days for the depression to become subclinical and the anxiety to reduce to moderate levels. However, even after 30 days of discontinued opioid use, there were still levels of mild anxiety and mild depression.94 Though the long-term effects on mental health are inconclusive, opioid usage can have an effect on mental health, especially during the withdrawal stage.
Medical Complications
If individuals with OUDAn addiction to opioids that is chronic and lifelong with serious potential consequences such as disability, relapse, and even death.6 OUD is listed in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) as a problematic pattern of opioid use leading to problems or distress.7 Physical dependence occurs within 4–8 weeks, much shorter than other substance use disorders. Ease of access is a notorious reason for the epidemic in the United States.8 OUD is typically measured through overdose rates versus the number of people it affects. “Opioid use disorder” is preferred over other terms such as “opioid abuse,” “opioid addiction,” or “opioid dependence.”9 disorder get sick or injured, they are more likely to have medical complications or a harder time recovering. In a study done on patients recovering from surgery, it was shown that when paired against individuals without OUD, 51.1% of OUD patients experienced complications, compared to 26.8% of the patients without OUD. They also experienced more adverse events (instances where the medical treatment administered resulted in further health complications), with 55% of OUD patients and 39.7% of non-OUD patients experiencing such events.95 When compared to the patients without OUD, the patients with OUD were more likely to leave the hospitals against medical advice.96 Leaving against medical advice can increase a patient’s likelihood of being readmitted in the future and can worsen health outcomes that could have been treated had they stayed in facilities.97 Research shows that people using illicit drugs, including people misusing opioids, incur injuries at approximately the same rate as people who are not using.98 However, when people with OUD do get injured, their risk of complications is heightened.
Suicide
Studies have shown that OUDAn addiction to opioids that is chronic and lifelong with serious potential consequences such as disability, relapse, and even death.6 OUD is listed in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) as a problematic pattern of opioid use leading to problems or distress.7 Physical dependence occurs within 4–8 weeks, much shorter than other substance use disorders. Ease of access is a notorious reason for the epidemic in the United States.8 OUD is typically measured through overdose rates versus the number of people it affects. “Opioid use disorder” is preferred over other terms such as “opioid abuse,” “opioid addiction,” or “opioid dependence.”9 can lead to increased rates of suicide, though the relationship between the two is sometimes unclear.99 This is in part because death from opioids can be a result of intentional suicides or accidental overdoses. It is often difficult to tell a person’s intention: in 2015, approximately 5.7% of the 52,400 drug overdose deaths in America were deemed “undetermined” in whether or not they were intentional.100, 101 About 10% were deemed intentional overdoses.102 Researchers have classified OUD itself as a risk of completing suicide.103 One theory explains that recurring opioid use can change the brain’s functions by altering a person’s perception of what their body needs to retain homeostasis and by tampering with the reward center of the brain. These changes often increase a person’s mental and emotional turmoil as they seek what their brain tells them they need, and that turmoil is a typical precedent to suicide.104 Studies have shown that among individuals with OUD, the rates of suicide are higher among women than men.105 This suicide risk among women with OUD is assumed to be in part due to the increased levels of chronic pain, mental health, and traumatic stress that women experience as opposed to men when involved in opioid use.106
Death
Opioids in the form of a pill or injectable opioids relieve pain and produce euphoria, but in turn, stimulate other physiological responses, such as slowed or stopped breathing, which can lead to death if taken in large doses.107 Drug overdose is the leading cause of accidental death in the United States, primarily from opioids as the most common drug.108 Of all 70,000 drug-related deaths that occurred in the United States in 2017, two-thirds (approximately 47,000) were opioid-related.109 Pain management experts believe that the high number of overdoses from opioids was not intentional but rather due to patients attempting to manage their unrelenting pain.110
From 2010–2020, the rate of opioid-related overdose deaths has increased by 225%.111, 112 One study illustrated how the rates change from year to year by looking at the overdose evolution from 2013–2014. In 2014, 47,055 drug overdose deaths occurred, with a one-year increase of 6.5% from 2013. The rate increased from 13.8 per 100,000 people to 14.7 per 100,000.113 This increase developed for both men and women, people aged 25–44 years and 55 years and older, non-Hispanic whites and non-Hispanic blacks.
Of adults aged 65 and older, rates of drug overdose deaths have increased from 2.4 to 8.8 deaths per 100,000 standard population between 2000 and 2020. This age group has lower death rates than other age groups but has increased significantly in the past 20 years.114 Nearly all age groups experienced increases in overdose death rates during 2015–2017, especially blacks aged 45–64 years and non-Hispanic whites aged 25–34 years.115
Practices
Medication-Assisted Treatment (MAT)
Although OUDAn addiction to opioids that is chronic and lifelong with serious potential consequences such as disability, relapse, and even death.6 OUD is listed in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) as a problematic pattern of opioid use leading to problems or distress.7 Physical dependence occurs within 4–8 weeks, much shorter than other substance use disorders. Ease of access is a notorious reason for the epidemic in the United States.8 OUD is typically measured through overdose rates versus the number of people it affects. “Opioid use disorder” is preferred over other terms such as “opioid abuse,” “opioid addiction,” or “opioid dependence.”9 remains a major issue in the United States, efforts to date to help those addicted have made no real headway. This is largely due to the lack of use of existing scientifically-proven tools and techniques, like evidence-based medications.116 According to the Substance Abuse and Mental Health Services Administration (SAMHSA), part of the US Department of Health and Human Services, the use of medication-assisted treatment (MAT) is a viable option for OUD recovery. MAT uses both FDA-approved medication and non-drug behavioral therapy to provide a “whole-patient” approach to recovery.117
This form of treatment aims to both help patients in their present recovery from OUDAn addiction to opioids that is chronic and lifelong with serious potential consequences such as disability, relapse, and even death.6 OUD is listed in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) as a problematic pattern of opioid use leading to problems or distress.7 Physical dependence occurs within 4–8 weeks, much shorter than other substance use disorders. Ease of access is a notorious reason for the epidemic in the United States.8 OUD is typically measured through overdose rates versus the number of people it affects. “Opioid use disorder” is preferred over other terms such as “opioid abuse,” “opioid addiction,” or “opioid dependence.”9, as well as promote sustained recovery over a long period of time.118 MAT is a series of prescription medications that helps normalize brain chemistry, block the euphoric effects of opioids, relieve cravings physiologically that are tied to the recovery period, and help normalize body functions. Medications that may be used to help achieve these effects are methadone, buprenorphine, or naltrexone.119 In addition to medication, behavioral therapy such as counseling, community-based services, family support systems, modifying behaviors that lead to opioid misuse, contingency management, and mutual help programs can be helpful depending on the individual’s needs.120
Impact
MAT has been shown to be clinically effective and to significantly reduce the need for detoxification services in an inpatient environment. It is able to address the needs of most patients by combining behavioral therapy and evidence-based medications.121 MAT is also able to improve patient survival, prevent overdose, decrease illicit use of opioids and criminal activity among people with OUDAn addiction to opioids that is chronic and lifelong with serious potential consequences such as disability, relapse, and even death.6 OUD is listed in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) as a problematic pattern of opioid use leading to problems or distress.7 Physical dependence occurs within 4–8 weeks, much shorter than other substance use disorders. Ease of access is a notorious reason for the epidemic in the United States.8 OUD is typically measured through overdose rates versus the number of people it affects. “Opioid use disorder” is preferred over other terms such as “opioid abuse,” “opioid addiction,” or “opioid dependence.”9, and increase the patient’s ability to maintain employment and retention in treatment.122 Compared to treatments not involving medications or no treatment at all, medications that treat OUD have been shown to decrease overdose risk by over 50% in many population-based studies.123
MAT significantly increases patient treatment adherence and reduces the illicit use of opioids compared with purely non-drug approaches or even purely drug approaches. In a study of OUD patients that took either methadone or buprenorphine/naloxone in treatment, they were able to abstain from heroin at a rate of 33.2% and 20.7% from all opioids for a period of 5 years.124 As a side benefit, MAT can also reduce the transmission of infectious diseases such as HIV and hepatitis C since the injection of opioids occurs less.125
Gaps
Although this form of treatment is highly effective, MAT remains difficult to access for all patients with OUDAn addiction to opioids that is chronic and lifelong with serious potential consequences such as disability, relapse, and even death.6 OUD is listed in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) as a problematic pattern of opioid use leading to problems or distress.7 Physical dependence occurs within 4–8 weeks, much shorter than other substance use disorders. Ease of access is a notorious reason for the epidemic in the United States.8 OUD is typically measured through overdose rates versus the number of people it affects. “Opioid use disorder” is preferred over other terms such as “opioid abuse,” “opioid addiction,” or “opioid dependence.”9. Many treatment centers for opioid and substance abuse do not provide MAT drugs. Of all publicly funded treatment programs in the US, only 23% reported offering any FDA-approved medications to treat OUD.126 Another barrier to MAT is limited insurance coverage and the lack of medical personnel qualified to distribute and facilitate medication use in recovery. The Affordable Care Act mandates insurance companies to pay for OUD treatment, but the benefits that are covered are not specified or are only covered for a specified amount of time.127 This limitation can cause harmful effects on patients seeking MAT treatment, oftentimes never receiving it at all. The amount of medical personnel that are eligible to provide and prescribe buprenorphine to treat OUD is too little for the number of patients with OUD in need of treatment. For 30 million Americans, the counties they reside in do not have any physicians with waivers that allow them to prescribe FDA-approved treatment medication for MAT.128 Providing greater access to MAT will be key to reducing OUD across the nation.
Preferred Citation: Holmgren, Macy. “Opioid Use Disorder in the United States.” Ballard Brief. April 2023. www.ballardbrief.byu.edu.
Viewpoints published by Ballard Brief are not necessarily endorsed by BYU or The Church of Jesus Christ of Latter-day Saints