Healthcare Access in Rural Communities in India
By Jacob Player
Published Fall 2019
Special thanks to Harper Forsgren for editing and research contributions
+ Summary
Rural communities in India face a severe shortage of access to healthcare services. There is little public spending on healthcare, and what money the government does spend is largely distributed to urban settings rather than rural ones. Additionally, the private healthcare industry primarily serves urban settings. While there is a significant healthcare personnel shortage throughout India, it is particularly problematic in rural areas. Because of this issue, those in rural areas seeking healthcare services must often travel distances of up to 100 km to access them. Healthcare providers that are serving rural communities are often local and have little to no formal qualifications or training. High rates of poverty are prohibitive to accessing healthcare for many rural communities; nearly 90% of the population is not covered by insurance, and a majority of costs are paid out of pocket or by taking out loans. In rural communities, there are significant disparities in important health indicators such as high rates of infant mortality, malnutrition, maternal mortality, low rates of vaccination, and low life expectancy. Current practices that are addressing this issue include the use of telemedicine, the formation of women-centric health clinics that are often mobile, the expansion of mini hospitals into less population-dense areas, and the creation of formalized training and accountability programs for local health providers.
+ Key Takeaways
- Rural communities in India suffer from a significant lack of access to healthcare. This lack of access results in high rates of maternal mortality, infant mortality, and malnutrition, as well as low life expectancy and low vaccination rates.
- This poor access to healthcare leads to a strong economic burden on the rural poor, and public spending and insurance companies have done little to mitigate it.
- This lack of access includes a severe shortage of qualified medical personnel, physical limitations such as distance, lack of established healthcare infrastructure, and inability to pay for necessary medical treatment.
- Current practices seeking to address this problem include the expansion of small hospitals into less populated areas, the formation of women’s health clinics, the use of technology to expand reach, and training programs for local healthcare service providers.
- The formation of women’s clinics and training local healthcare providers have demonstrated significant impact through randomized control trials, whereas other current practices have reported outcomes but have yet to provide conclusive data demonstrating impact.
+ Key Terms
Rural—The definition of rural varies significantly by location and measurement group; general trends include a low population density, a low community structure, and a high proportion of the male working population involved in agriculture. In India, the National Sample Survey Organization (commonly used in studies) defined rural as:
- An area with a population density of up to 400 per square kilometer
- Villages with clear surveyed boundaries but no municipal board
- A minimum of 75% of male working population involved in agriculture or related activities1
Primary Care—Medical care by a physician or healthcare professional who is the patient’s first contact with the healthcare system.2
Out-of-pocket costs—Expenses that are paid for directly by an individual or family without financial assistance or insurance.3
Socioeconomic status—An individual’s position within the social ladder, dependent on several variables including occupation, education, income, wealth, and place of residence.4
Hardship financing—Paying for something only by taking out a loan with interest or by selling one’s possessions.5
Herd Immunity—A condition that results when a significant percentage of a population (typically 90-95%) is immune to a disease, typically as a result of vaccination, preventing the spread of the disease through the population to non-immune individuals.6
Wasting—The loss of healthy muscle and fat tissue, typically associated with increased physical frailty and reduced mental alertness, and generally accompanied by arrested development in children.7
Life Expectancy—The anticipated number of years an individual or group will live, often affected by a variety of factors such as genetics or disease.8
Telemedicine—The delivery of healthcare services, where distance is a critical factor, by all healthcare professionals using information and communication technologies to exchange valid information for diagnosis, treatment, and prevention of disease and injury.9
Context
Good public health is essential to the proper functioning of society. Common health indicators such as nutrition, infant mortality, life expectancy, and so on provide important insights into the overall well-being of a given population. Having adequate access to proper healthcare is a multi-faceted dilemma that can contribute largely to disparities in healthcare received. In India, a significant dividing line in healthcare access can be drawn between rural and urban communities. Approximately 75% of health infrastructure and resources are concentrated in urban areas, where only 27% of the population resides.10
As of 2017, nearly 900,000,000 Indians were still living in rural communities.11 Rural India experiences higher rates of infant mortality and anemia, as well as lower birth weights, immunization rates, and rates of healthcare service use than urban Indian communities.12 Women in particular suffer poorer health outcomes due to lack of access to maternal and reproductive care, cultural taboos and stigmas, and lower familial priority in the face of cited prohibitive healthcare costs.13
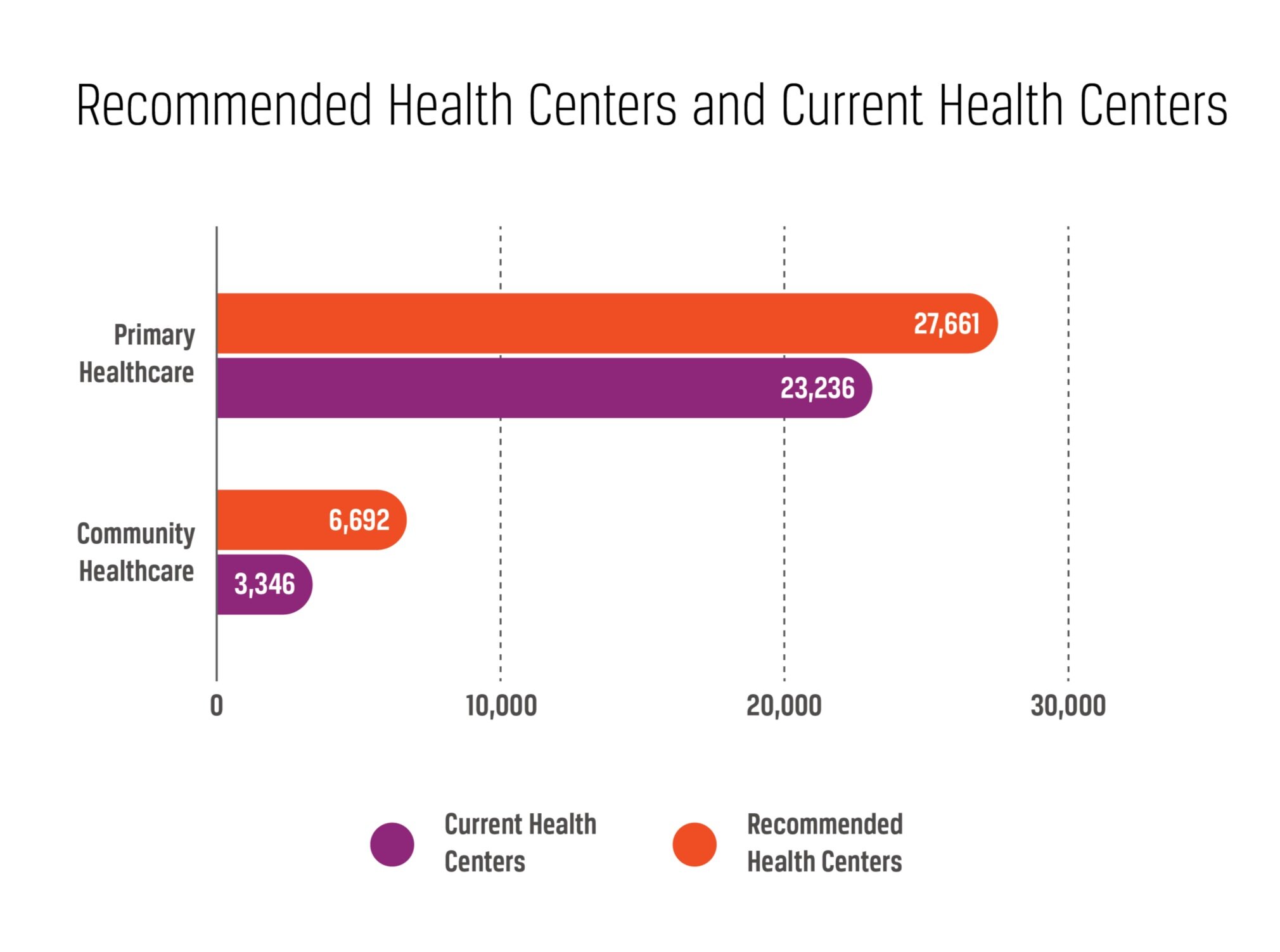
The public healthcare system in India is divided into primary, secondary, and tertiary facilities with decreasing specialization and population size served from primary to tertiary. In rural areas, primary health services are provided through subcenters, primary health centers, and community health centers meant to handle health needs at the most basic level for populations of 3000–5000 individuals.14 When compared to the Indian government’s defined standards, India is 16% below the number of primary health centers and approximately 50% below the number of community health centers it should have,15 and lower health indicators in rural communities are a direct reflection of this poor healthcare access.
Approximately 86% of medical visits in India are from individuals living in rural areas, with a majority traveling over 100 km to reach available healthcare facilities, and where 70-80% of the cost is paid out-of-pocket.16 Although poverty already has a negative effect on health, poverty in rural areas has been shown to have even greater negative effects than poverty in urban areas.17 Additionally, many measures of disease prevalence are underreported because of the difficulty associated with collecting data in rural areas, and because impoverished individuals are less likely to report things they perceive as negative about themselves. This fact suggests routine underdiagnosis and underreporting among India’s poor, when compared to diagnostic or standard methods of measurement.18
Contributing Factors
Socioeconomic Barriers
The ability to pay for healthcare is a significant hurdle for those in rural India. In Orissa, one of India’s poorest states, 25% of households that had any healthcare costs, and 40% of households that experienced a hospitalization, had to take out loans or sell assets to pay for healthcare costs out-of-pocket.19 In total, only 17% of health expenditure is borne by the state, with 82% out-of-pocket,20 making it the sixth lowest country in the world for public health spending. Although women generally have far worse health outcomes than men, these trends disappear or are reversed when controlled for economic independence,21 indicating that financial inequality plays an important role in poor women’s health. Low socioeconomic status has been correlated with lower healthcare access as well as lower utilization of better qualified healthcare providers.22 Poor healthcare access greatly decreases the use of preventative care, which for many undercovered preventative treatments in India, such as vaccination, can result in more severe future health problems. These problems increase the overall cost of healthcare and decrease a population’s overall number of years in perfect health.23
Qualified Personnel Shortage
India suffers from a severe lack of qualified healthcare professionals in rural areas. Compared to established guidelines, as of 2015, 8% of primary health centers were without a doctor, 38% without a lab technician, and 22% without a pharmacist. Community health centers had an astonishing 83% vacancy for surgeons, 76% for gynecologists or obstetricians, 83% for physicians, and 82% for pediatricians.24 Among healthcare providers in India, the number of informal providers with highly variable levels of education and training greatly outnumber those with valid medical qualifications. Although these informal providers render important services where they would otherwise be absent, qualifications and training can also vary widely with location, and inappropriate prescriptions of drugs is common.25 One study found that 67% of healthcare providers reported no medical qualifications whatsoever. Furthermore, when comparing formally trained medical providers to those without training, only “small differences” were found between the two, overall “correct diagnoses were rare,” and incorrect treatments were “widely prescribed.”26 All quality metrics have been found to be higher in private clinics than in public ones,27 suggesting disparities in training that follow socioeconomic boundaries. Lack of economic opportunity and a shortage of qualified professionals has led to higher concentration of trained medical professionals in cities and in private practices, with fewer qualified professionals serving rural areas.28
Infrastructure Problems
Many disparities can result from a lack of well-established businesses, branches of government, or other organizations that have critical mass and provide necessary auxiliary services. Although private sector healthcare systems are generally better funded and regarded as providing an improved quality of care, they remain largely underdeveloped and serve primarily urban locations. Few business ventures have attempted to find economical market solutions to providing improved healthcare access in rural communities.29 There is also little framework for maintaining health records for patients, meaning that valuable long-term data for diagnosis and patient health history is largely missing, reducing informed and effective treatment as well as the ability of a provider to track individual patient care over an extended period.30
Many healthcare experts in India are critical of the lack of government healthcare expenditure, which is less than 1% of India’s Gross Domestic Product (GDP),31 and of the fact that this funding is spent primarily in urban areas where only a minority of the population resides. Regionally this problem is magnified, as there is little national-level health intervention, and health financing is heavily dependent on funds from individual states, which mirror the boundaries of socioeconomic inequality between urban and rural areas. Additionally, there are few insurance plans available; all public and private insurance plans together cover only roughly 11% of the population, leaving the rest to pay out-of-pocket or through hardship financing.32 As previously noted, many rural inhabitants have to travel distances upwards of 100 km to access healthcare services, frequently on dirt roads that make travel difficult and thus reduce the likelihood of receiving medical care when compared to areas with more paved roads.33 Inadequate means of transport for ill individuals and roads that are poorly maintained further complicate access to quality healthcare services.34
Consequences
Financial Burden
Healthcare expenditures are believed to be one of the greatest causes of impoverishment in India. The costs associated with healthcare are one of the primary contributing factors to dropping below the poverty line. One study estimated that in 2004 over 63 million individuals in India were pushed to below-poverty-level due to healthcare expenditures.35 This number is equivalent to 7.6% of the nation’s households falling below poverty level due to healthcare expenses in a single year. The study also suggests that after Pakistan, India had the highest rate of out-of-pocket health expenditures in the world.36 Financial strain may also have other detrimental effects on health such as increasing stress, something that has the potential to create or exacerbate many health problems.37 Additionally, financial burden may also decrease the likelihood of seeking necessary preventative healthcare services in the future, which can lead to untreated health problems becoming even more severe. The costs of receiving adequate healthcare in rural India are sufficient to impoverish otherwise financially solvent families and to increase the debt of the already destitute to a point beyond feasible mitigation, with one study finding that the number of Indians pushed below poverty level by healthcare costs was more than 3 times greater in rural areas than in urban areas.38
Maternal Mortality
Poor healthcare access in rural India includes little access to natal, post-natal, and reproductive care, greatly reducing the likelihood of having trained medical personnel present before, during, or after the pregnancy or birth in the event of complications, or of expectant mothers receiving potentially life-saving maternal education or training. One study in northern India found that maternal death rates make up 21.4% of total deaths.39 Total maternal mortality was 230 deaths per 100,000 live births, with major causes being hemorrhage (18.2%), sepsis (16.4%), anemia (16.4%), abortion (9.1%), and obstructed labor (7.3%).40 Maternal death greatly contributes to decreased average life expectancy in a population and further imposes strain on young families and local communities to provide for the basic needs of its members. Maternal death has significant effects on proper childhood development and can further compound negative psychosocial and physiological health outcomes for a family. One study from 1997 found that maternal death in India doubled the chances of premature death for surviving sons and quadrupled the chances of death for surviving daughters.41 For families in poverty that are obligated to work daily for sustenance, maternal death likely means leaving children with no adult supervision whatsoever, increasing their likelihood of negative health outcomes and death.
Infant or Child Mortality
Poor neonatal and pediatric care has had devastating consequences on mortality rates in India. An estimated 881,995 children less than 5 years of age died in India in 2017.42 Mature and adult children play an important role in maintaining, caring for, and providing for the physical needs of a family unit in close-knit rural communities, and early death precludes their ability to help. Furthermore, premature death represents a lost emotional, physical, and financial investment associated with sustaining a child through pregnancy and infancy that could have otherwise benefited the family had the child lived through adulthood.43 Additionally, the emotional strain associated with the loss of a child can increase the stress experienced by members of a family, increasing their risk of a myriad of negative stress-related health consequences.
Low Vaccination Rates
Vaccination is an essential intervention to reduce the prevalence of serious and life-threatening diseases, especially among young children. Approximately 50% of eligible children in India have received essential vaccinations, and there is significant inequality in vaccination coverage, with the lowest rates associated with a number of causes including area of residence, rurality, and low access to health services and other infrastructure.44 Although vaccination rates vary widely with region (from 25.2% to 57.7%), rurality is always associated with decreased coverage.45 Many vaccine-preventable diseases are highly contagious and can frequently result in disability and death,46 especially in the absence of proper healthcare facilities. Additionally, areas surrounding India, such as Pakistan, are known for resisting vaccine use,47 further increasing risks. With low rates of local vaccination, communities are unable to establish the significant benefits of herd immunity that can act preventatively against the spread of these diseases, meaning that the infection of a single individual can potentially have devastating consequences for an entire local community.
Malnutrition
Malnutrition is a serious health condition that can result in fatigue, lost productivity, poor mental alertness, and reduced life expectancy in adults; in children it can lead to permanent health issues such as stunted growth, permanent physical impairment, infection, and even death. Among the various factors affecting malnutrition in childhood, use of healthcare services is one of the most important, showing even greater effects than per capita income.48 Healthcare services provide essential education on proper childhood nutrition as well as growth monitoring services that act to combat malnutrition. Without this oversight, these negative effects can significantly impact individuals’ future health and productivity in their community, potentially deepening its economic burden. The Food and Agriculture Organization of the United Nations estimates that 22% of India’s population is undernourished.49 One study found that 36% of women and 34% of men aged 15-49 were found to be below the internationally accepted Body Mass Index (BMI).50 The negative effects of malnutrition in children are even more far-reaching: stunted growth has been found to affect 48% of Indian children under the age of 5, while 19.8% of children under 5 are affected by wasting, and 42.5% of children under 5 are underweight, which is the highest rate in the world.51 These rates are even worse in rural areas when compared to urban areas.52
Life Expectancy
Life expectancy relates directly to healthcare access, as early childhood death, death resulting from injury, and even preventable death of the elderly all affect the average lifespan of a person. These problems can be reduced with sufficient healthcare access. Average life expectancy of a population can be understood as a useful measure of overall population health. Life expectancy in India shows significant variation between urban and rural regions; rural areas show a lower life expectancy than urban areas, with an average rural lifespan of 61.75 years, more than 10 years shorter than the average urban lifespan.53 Low life expectancy has widespread economic effects. Younger populations have fewer productive years in skilled or specialized labor as well as a higher workforce turnover. These effects can impede economic growth and the technological and societal benefits derived from specialization and skilled labor.
Practices
Telemedicine
Telemedicine uses electronic information communication technologies to provide support and healthcare for individuals separated by distance. This innovation has the potential to help decrease the gaps in available and qualified health personnel between rural and urban areas, as well as to provide new market opportunities to expand healthcare towards rural communities. Telemedicine hardware typically includes a computer, scanner, printer, and videoconferencing equipment, which enables the acquisition of patient information and communication from health providers. Benefits of telemedicine include:
- Reduction in time and costs of patient transportation
- Critical care monitoring when it is not possible to transfer patients
- Improved opportunities for medical education and research
- Opportunities to provide qualified medical care where otherwise unreachable
- Improved disease tracking ability54
Many different groups are currently pursuing or supporting telemedicine in India, including many efforts by the Indian government. Notable groups include the Indian Space Research Organization (ISRO), as well as some private sector companies such as TeleVital and Kria; there is often significant collaboration between these companies. Organizations pursuing this approach seek to find ways to set up and establish contacts or work-sites between rural and urban areas for these communications to take place. Telemedicine also enables doctors to maintain training and professional competence by continuing to reside in urban locations where medical knowledge is more readily accessible. Additionally, telemedicine seeks to expand the influence of medical specialists to more remote regions focused on primary care.
Impact
Studies on the effectiveness of telemedicine have been primarily limited to reports in terms of outputs or outcomes only. Initial government-sponsored implementation in partnership with the ISRO and use of their satellites has successfully connected 22 highly specialized hospitals with 78 rural and remote hospitals across the country. Although implementation is still recent, initial reports have been made of lives saved through Telemedicine-guided surgery. Through this system, approximately 25,000 patients have been provided with teleconsultation and treatment.55 Some preliminary data suggests significant cost saving for patients due to elimination of travel and lodging expenses.56 In Tripura, where telemedicine has been implemented in 20 hospitals, crude birth rate and female literacy rate have seen significant advancements; however, this observation has not been controlled for and may well be attributable to other factors.57 A review of studies on the impact of telemedicine found that of 41 hospitals that used randomized control trials to analyze clinical outcomes, 39% reported significant improvements.58
Gaps
Funding for telemedicine in partnership with the government faces possible future restrictions, potentially limiting access for rural populations to a significant degree. Studies on the cost effectiveness of telemedicine are currently limited, and some but not all have demonstrated a reduction in associated healthcare costs.59 Research on the economic benefits of telemedicine largely lack randomized control trials, adequate sample size, and appropriate measurements. Little quality impact data exists on the implementation of telemedicine, with most studies citing either potential benefits or outcomes only. This lack is possibly due to the relatively new implementation of telemedicine; however, there are significant reviews that critique the scientific rigor of impact studies that have been performed,60 suggesting methodological problems rather than time may be a limiting factor. There are potential financial motivations that may also contribute to a negligence towards quantitative data collection and conflicts of interest. Impact data from a private industry telemedicine venture has shown that intervention did not significantly improve rates of appropriate disease treatment, disease prevalence, or healthcare outcomes for childhood diarrhea and pneumonia.61 Additional private sector impact data has shown that both provider participation in telemedicine as well as use among target populations are low. Telemedicine still faces some logistical difficulties in establishing itself in truly rural communities and faces limitations in access to individuals capable of providing intensive treatment in the event of need. Some preference has also been shown by rural patients for seeking care from providers without qualifications, even with telemedicine readily available.62
Training Local Healthcare Providers
This approach seeks to make use of existing untrained medical providers by educating them to appropriately identify and treat common illnesses, such as pneumonia and diarrhea. Existing local entrepreneurs that are attempting to furnish medical services provide a pre-made framework for a developing healthcare system. This approach seeks to enlist, hire, or partner with existing rural healthcare providers and provide them with basic training and supplies to increase their efficacy, improve local industry, offer oversight, and provide points of contact for more serious medical concerns to be treated. This method aims to significantly reduce the gravity of the most common illnesses, reduce potential harm caused by malpractice, and provide improved medical education directly to the communities most in need.63 One well-established example of this intervention is the Society for Education, Action, and Research in Community Health (SEARCH),64 which trains community health workers and deploys mobile medical units in rural and impoverished areas, conducts research, and advises public policy, although many community health worker interventions operate without public sector involvement.
Impact
Single-blind randomized controlled trials have been conducted on training programs for informal providers in India that consisted of 72 sessions of training over a 9 month period. Average attendance at training sessions was 56% with no control group contamination. Providers that received training were determined to be 15.2% more likely to adhere to condition specific checklists than control groups. Correct case management increased by 14.2%, and patient caseload increased from 7.6-17.0%. Training had no effect on unnecessary medicine and antibiotic use.65 Additional studies have shown that community intervention trainings increased safe child deliveries and reduced neonatal mortality.66 A retrospective study on a community-based primary health training program showed that, in project communities, hazard of death in children under 5 years of age had been reduced by 30% after the neonatal period when compared to control villages, and there was no significant difference in hazard of death during the neonatal period.67
Gaps
Some health indicators have consistently remained low despite local training program interventions. Significant variations and levels of success occur between villages and programs, and no standardized or dominant program has yet been developed or employed broadly. Impact has been shown to vary widely with community attitudes concerning the specific interventions used.43 Encouraging significant participation in these programs and implementation afterwards poses a unique challenge to this approach. Establishing contact with rural communities can be difficult and longevity of the effect of interventions has yet to be determined.
Targeted Development of Private Hospitals in Small or Medium Sized Communities
Social entrepreneurs in the healthcare community have found profitable means of bringing healthcare more directly to rural areas. Focuses have been on building small hospitals in semi-urban areas next to public transport hubs and scaling down operations to be appropriate for the size of the communities they serve in order to stay profitable. To combat doctor shortages and competition, mini-hospitals target recent medical graduates with offers of senior positions rather than the low starting positions anticipated at larger urban hospitals, as well as a corresponding competitive increase in pay. By reducing operating costs with smaller hospitals closer to rural communities and providing financial incentives to overcome staffing issues, this method hopes to build sustainable infrastructure to reach underserved communities by bringing the hospitals to them.68 This method is the approach pioneered by Vatsaalya Healthcare,69 which is currently operating 8 hospitals throughout India and seeking to expand. By deliberately targeting the locations of their healthcare centers they have been able to reduce the distances required to travel for their services, with 30% of patients coming from within a 5km radius and 70% traveling no more than 30–40km70, effectively halving the distance most rural Indians have to travel. Small hospitals hope to develop lasting and valuable infrastructure as well as create further training opportunities and economic growth in disadvantaged rural communities.
Impact
Small private hospitals have proven to be economically viable and are likely to inspire more widespread adoption and the growth of related healthcare industries in semi-rural locations.71 Available studies have largely centered around proving the economic feasibility of small hospitals. One study concluded that basic hospital services can be added effectively to other available health services with little increase in total costs, and significant accruing benefits from reduction in disability or death causative illness prevention.72 One hospital network reported outcomes of establishing 9 hospitals in unserved towns, serving approximately half a million customers annually and over 3 million individuals since inception.38 Patient costs for certain procedures such as child delivery are purported to have been successfully decreased by as much as 300% using an income-based 3 tier cost approach. Small private hospitals have provided over 500 additional beds to rural communities and continue to grow with network expansions. Small hospitals have also provided small community outreach programs, including mobile health camps that claim to service an additional 3000 individuals per month, as well as community health education programs for children that claim to reach at least an additional 3000 individuals per month.73
Gaps
Impact studies on the expansion of small hospitals in rural areas are highly limited. Due to the economic self-sufficiency of this approach and its practice almost exclusively in the private sector, there is relatively little pressure to conduct impact research studies in comparison with social ventures that seek public funding. Reported data largely focused on outcomes. Additionally, many of these outcomes are self-reported, potentially biasing the data, and many outcomes are reported in vague terms, such as patients seen, which provide little insight into differential health outcomes due to hospital intervention. Expansion of small private hospitals is still a relatively new practice, and could potentially face public sector competition or regulation as it continues to expand. Even with outside investment, the creation of hospitals and recruitment of new physicians is a slow approach. Further possible limitations include decreasing financial viability as hospitals become increasingly rural, as well as the ability to effectively reduce distances from rural communities.
Forming Women’s Clinics or Divisions
This approach seeks to overcome differential health outcomes by primarily focusing on women. There are substantial cultural taboos concerning women and women’s rights to overcome in rural India, and few resources available for them specifically. Many health indicators such as maternal health, infant mortality rates, and STD transmission relate directly to women but remain unaddressed due to taboo or lack of education. Groups using this approach seek to establish cost-effective clinics in rural areas that establish precedents of regular female care, comfortable opportunities to ask questions about sexual health, and education concerning STDs and proper childcare. Other proponents use existing clinics in underserved areas provided by outside funding and establish personnel trainings or specific staff positions focused on female care, and then coordinate for them to be held accountable for health outcomes by local community leader oversight.74
Impact
A non-blind randomized control trial showed that in 2 groups that both received health services and had trained birth attendants, the formation of a women’s support group for mothers independently reduced neonatal death from 36.5 deaths per 1000 births to 33.9 deaths per thousand births.75 Another study showed that when women’s groups were formed and led by a female facilitator that helped identify and address perinatal problems, neonatal death decreased from 36.9 per 1000 births to 26.2 per thousand births, and maternal death rates decreased from 341 per 100,000 livebirths to 69 per 100,000 livebirths. Rate of stillbirths remained unchanged between control and trial groups.76 Women-centric health intervention screenings such as visual inspection for cervical cancer incidence have also shown to increase treatment of potentially life-threatening conditions.77
Gaps
Cultural attitudes have been shown to directly influence participation with female-health specific intervention strategies. Likelihood of participation has been shown to decrease with age, lower education, and former contraceptive use. Additionally, likelihood of complying with treatment has been shown to decrease with lower education, increased number of previous pregnancies, and unmarried status.78 It is also unclear if women’s health groups successfully change cultural perceptions of female reproductive care. Additionally, interventions that require trained healthcare professionals are likely to face similar staffing shortages as normal rural medical efforts. Although improvements have been verified in women’s groups as statistically significant, differences have been shown to be relatively small and may not always be practical for the resources available compared to other intervention options.
Preferred Citation: Player, Jacob. “Healthcare Access in Rural Communities in India.” Ballard Brief. December 2019. www.ballardbrief.org.
Viewpoints published by Ballard Brief are not necessarily endorsed by BYU or The Church of Jesus Christ of Latter-day Saints